It started with what seemed like a harmless goal—just a little weight loss, a few pounds here and there. Sarah, a 32-year-old marketing executive, had never thought of herself as someone with an eating disorder. She just wanted to feel better in her clothes, move more comfortably, and, if she was honest, finally fit into the version of herself she thought she was supposed to be.
When she heard about Ozempic, a medication originally developed for diabetes but increasingly prescribed for weight loss, it seemed like the perfect solution. “It curbed my appetite so much that I barely thought about food,” she admitted. At first, she felt empowered—watching the scale drop, hearing compliments from friends. But soon, something shifted. She began skipping meals, not because she was consciously restricting but because she simply never felt hungry. The thought of eating became almost repulsive. Even when her energy lagged and her hair began to thin, she brushed it off.
By the time she recognized something was wrong, Sarah’s weight loss had turned into something else entirely—something that looked a lot like an eating disorder.
When Healthy Habits Become Harmful
Eating disorders don’t always look the way we expect them to. They don’t come with a single body type, gender, or age group. And more often than not, they don’t start with the intention of developing one.
Many people, like Sarah, begin their journey with what seems like a wellness goal—to be healthier, to manage their weight, to take control. But in a world where thinness is celebrated and food is feared, the line between “healthy eating” and “disordered eating” can become dangerously blurred.This is especially true with the rise of weight loss injectables like Ozempic, Wegovy, and Mounjaro. These medications have given countless people a way to manage their health, but they have also opened the door to a new form of restriction, one that can silently mimic or exacerbate eating disorders.
What Are Eating Disorders?
At their core, eating disorders are not about food—they are about control, self-worth, and mental health. While they manifest in different ways, they all share one dangerous trait: a disordered relationship with eating and body image.
Types of Eating Disorders & Their Hidden Dangers
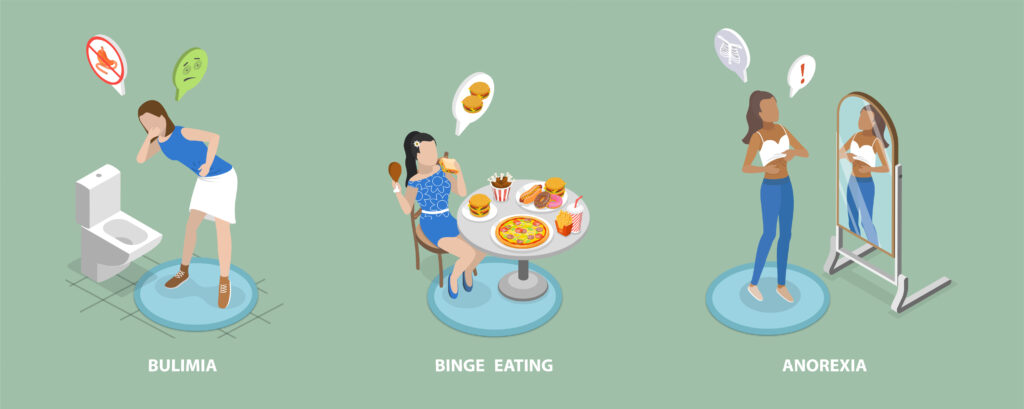
Anorexia Nervosa – The severe restriction of food due to an intense fear of weight gain and a distorted body image. It carries the highest mortality rate of any psychiatric disorder, often leading to heart failure, osteoporosis, and organ damage.
Bulimia Nervosa – A cycle of binge eating followed by purging (vomiting, laxatives, excessive exercise). It can cause severe electrolyte imbalances, heart arrhythmias, and digestive damage.
Binge Eating Disorder (BED) – Recurrent episodes of eating large quantities of food, often rapidly and in secret, without purging. This can lead to diabetes, high blood pressure, and severe emotional distress.
Avoidant/Restrictive Food Intake Disorder (ARFID) – A severe avoidance of certain foods due to sensory sensitivities, fear of choking, or past trauma. Unlike anorexia, ARFID is not driven by body image concerns, yet it leads to malnutrition and extreme weight loss.
While these conditions are different, they all pose serious health risks. But here’s what many people don’t realize: not everyone with an eating disorder looks underweight. In fact, many are in “normal” or larger bodies, making their struggle easier to dismiss—by doctors, by family, and even by themselves.
When Weight Loss Becomes Dangerous
At first glance, weight loss injectables seem like a medical breakthrough. And for some, they are. When used properly under medical supervision, they can help manage diabetes, heart disease, and obesity-related conditions.
But what happens when these medications are used not as a health tool, but as a shortcut to thinness?
For some, like Sarah, the complete loss of appetite becomes an unintended reinforcement of restrictive eating habits. What starts as a way to lose weight turns into a struggle to remember to eat at all.
For others, the fear of regaining weight after stopping the medication leads to extreme food avoidance, compulsive exercising, or prolonging use of the drug even when it’s no longer medically necessary.
This is where the problem lies. If we measure health purely by the number on the scale, we ignore the mental and physical damage happening beneath the surface.
The Warning Signs: Who’s at Risk
Eating disorders thrive in secrecy. The people struggling often don’t even recognize their behavior as harmful. That’s why it’s important to know the signs:
🚩 Skipping meals or constantly “forgetting” to eat
🚩 Extreme fear of hunger returning
🚩 Frequent trips to the bathroom after meals (a potential sign of purging)
🚩 Obsessing over weight loss, food labels, or calorie counting
🚩 Sudden changes in weight—both loss or gain
🚩 Avoiding social situations that involve food
🚩 Exercising excessively, even when exhausted or injured
If you or someone you know is exhibiting these behaviors, it’s time to seek help.
How to Help Someone Who’s Struggling

Sarah didn’t think she had a problem. She thought she was just “taking control.” But when her best friend gently asked, “Hey, I’ve noticed you haven’t been eating much lately. Are you okay?” it was the first time she considered that maybe, just maybe, this wasn’t normal.
If you suspect someone in your life is struggling, approach them with kindness, not judgment:
“I care about you, and I’ve been worried. Want to talk?”
“I’ve noticed some changes in the way you eat, and I just want to make sure you’re okay.”
“You don’t have to go through this alone. There are people who can help.”
Encouraging professional support is crucial. A therapist, dietitian, or doctor specializing in eating disorders can provide treatment options that address both the physical and mental aspects of recovery.
📍 Where to Find Help:
🆘 National Eating Disorders Association (NEDA): www.nationaleatingdisorders.org
📞 NEDA Helpline: 1-800-931-2237
Shifting the Conversation: Health Over Thinness
Sarah’s story isn’t unique. It’s happening everywhere—in conversations between friends, in weight loss ads, in doctors’ offices where weight is prioritized over well-being.
As weight loss medications continue to rise in popularity, we must ask ourselves: Are we prioritizing true health, or just chasing a thinner body at any cost?
This National Eating Disorders Awareness Week, let’s challenge the toxic belief that weight equals worth. Let’s recognize that health includes mental and emotional well-being, not just a number on a scale. And let’s support each other in finding balance, not extremes.
Because no one should have to struggle in silence. And no one should have to choose between weight loss and their well-being. 💙