When we talk about the “biological clock,” the conversation often centers on women. It’s widely understood that female fertility declines with age and that pregnancy risks increase for older mothers. But what about men? Can age impact male fertility and the health of their future children?
The answer is yes, though male fertility declines differently than female fertility. While men don’t experience a menopause-like event, their reproductive potential is not immune to aging. In fact, medical experts recommend that men over 40 be counseled on the potential risks associated with fathering children later in life.
As a healthcare professional, I see many patients unaware that age-related changes affect both parents in a pregnancy. While a woman’s egg count and quality decline significantly with age, men also experience biological aging of their sperm, which can lead to genetic mutations and potential health risks for their children, explains Dr. Kendra Segura, MD, MPH, FACOG.
What Is Advanced Paternal Age?
Unlike female fertility, which has a clear decline after 35 and a near halt after menopause, male fertility declines more gradually. However, there is no universal consensus on when a man becomes an “older father.”
The American Urological Association (AUA) and the American Society for Reproductive Medicine (ASRM) in a joint statement advised that men aged 40 and older should be informed of the potential risks to their future children. At this point, the chances of sperm abnormalities, genetic mutations, and pregnancy complications begin to rise.
How Does Age Affect Male Fertility?
While men can produce sperm well into their senior years, sperm quality does not remain constant. Several biological changes occur as men age:
- DNA Damage and Mutations: Sperm is constantly produced, and with each new cycle, errors can occur in DNA replication. These errors accumulate over time, increasing the risk of passing genetic mutations to offspring.
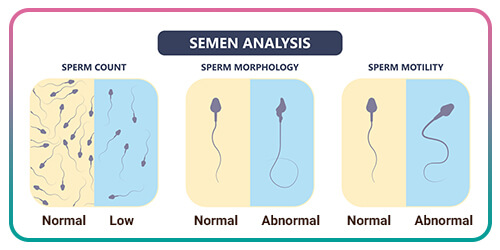
- Reduced Sperm Motility: Older men tend to have sperm that swim more sluggishly, making conception less likely.
- Lower Sperm Count: The overall number of sperm produced declines with age, reducing fertility.
- Hormonal Changes: Testosterone levels gradually decrease over time, which can impact libido, erectile function, and sperm production.
Think of sperm like a copy of a copy of a copy, says Dr. Kendra. Over time, errors accumulate, and while one or two small mistakes may not have a huge impact, a large accumulation of mutations can increase the risk of developmental disorders in children.
Health Risks for Children of Older Fathers
Several studies have shown that children born to fathers over 40 have an increased risk of neurological, psychiatric, and genetic conditions due to DNA mutations in sperm. These risks include:
- Autism Spectrum Disorder (ASD): A 2017 study published in JAMA Psychiatry found that fathers over 40 were more likely to have children diagnosed with autism compared to younger fathers. This is believed to be linked to genetic mutations in sperm that affect brain development.
- Schizophrenia and Mental Health Disorders: Research suggests that older paternal age is associated with a higher risk of schizophrenia and bipolar disorder in offspring. The exact cause is still being studied, but scientists believe it is linked to age-related changes in sperm DNA.
- Rare Genetic Conditions: Older fathers have a higher chance of passing on genetic mutations linked to disorders such as achondroplasia (a type of dwarfism) and other rare conditions caused by spontaneous mutations in sperm.
- Increased Risk of Miscarriage: While maternal age is a well-established factor in miscarriage, paternal age plays a role as well. Sperm DNA fragmentation, which increases with age, has been linked to a higher risk of miscarriage and failed pregnancies.
How Does This Compare to Women’s Biological Clock?
While both men and women experience reproductive aging, the impact is more gradual for men and more abrupt for women.
- Women are born with a finite number of eggs, and fertility declines rapidly after 35. By menopause, natural conception is no longer possible.
- Men continue producing sperm throughout life, but quality declines over time, leading to higher risks of genetic disorders in children.
We always talk about a woman’s age in fertility conversations, but the father’s age is equally important. It’s not just about being able to conceive—it’s about ensuring healthy sperm that leads to a healthy pregnancy and child.
What Can Men Do to Improve Reproductive Health?
For men planning to father children later in life, proactive steps can improve sperm health and reduce risks:
- Maintain a healthy lifestyle with a balanced diet, regular exercise, and by avoiding smoking and excessive alcohol consumption
- Manage stress and sleep, as chronic stress and poor sleep disrupt hormone balance and impact sperm production
- Avoid excessive heat exposure, such as frequent use of hot tubs, saunas, or tight clothing, which can impair sperm production
- Get regular health screenings to monitor testosterone levels, sperm quality, and overall reproductive health
- Consider genetic counseling to assess risks before trying to conceive
Final Thoughts: Should Men Be Concerned About Their Biological Clock?

Yes, while the decline in male fertility is less abrupt than in women, it does happen. Aging fathers have increased risks of passing on genetic mutations that can impact their children’s health. If you or your partner are considering pregnancy later in life, a conversation with a healthcare provider can help assess risks and optimize reproductive health.

