Have you ever found yourself forgetting where you left your keys, or struggling to recall someone’s name in the midst of a busy day? Momentary lapses in memory happen to all of us, but as we grow older, it’s only natural to become more concerned about maintaining sharp cognitive function. We already know that blood pressure, stress, exercise, and diet play major roles in our overall health as we age. But what if there’s more to it? What if “good” cholesterol—something you might only associate with heart health—has a deeper, more direct impact on your brain than previously imagined?
A groundbreaking study from UT Southwestern Medical Center has shed new light on how high-density lipoprotein (HDL), often called the “good” cholesterol, might help preserve healthy brain matter in middle-aged adults. When most of us think of cholesterol, we picture a dreaded lab value that needs to stay low to keep us healthy. But not all cholesterol is created equal! HDL is often touted for its beneficial effects on heart health, and now it seems that those benefits might also extend to the brain in ways we never fully appreciated before.
Let’s dive deeper into the significance of this research, look at what the experts from UT Southwestern discovered, and talk about what it means for you, your family, and your loved ones—particularly if you’re middle-aged or heading that way. As a nurse practitioner who has worked both in the fast-paced environment of the ER and in a family medicine clinic, I’ve seen firsthand the difference that good preventative care can make. In the emergency department, I’ve treated patients who’ve come in with strokes or heart attacks—often related to long-standing issues with cholesterol and blood pressure. In family medicine, we focus on preventing such issues, providing education, and encouraging lifestyle changes. This new research has me more excited than ever about empowering patients to take control of their health and protect their precious noggins!
The Study at a Glance
Researchers at UT Southwestern assessed 1,826 participants between the ages of 35 and 70, all enrolled in the multiethnic, population-based Dallas Heart Study—a well-known longitudinal study that is now in its 25th year. The participants’ lipoprotein concentrations (including various types and sizes of HDL particles) were measured using advanced nuclear magnetic resonance. Then, the participants underwent cognitive function testing and brain magnetic resonance imaging (MRI) to measure their gray matter volume.
What did the team discover? Quite a bit! The study suggests that it’s not just about having enough HDL in your blood—it’s about the function of those HDL particles, especially the smaller ones. Higher concentrations of small-particle HDL were linked with greater gray matter volume in the brain and better cognitive abilities. This is huge because, historically, doctors and researchers have sometimes been stumped by how exactly HDL (the “good” cholesterol) is related to brain health—some studies showing benefits, some showing little to no effect, and some even showing conflicting results. However, by looking at small HDL particles and how they function, this research team was able to reveal a potential new way to measure and protect cognitive health in adults.
Why Does Gray Matter Volume Matter?
If you’ve ever heard someone use the phrase “use your gray matter,” they’re talking about the neurons in your brain’s cortex that handle critical functions such as muscle control, sensory perception, memory, emotions, speech, decision-making, and self-control. In simpler terms: gray matter is where a lot of the “thinking” happens. Studies have shown that reduced gray matter volume, or the shrinking of these areas, can be linked to cognitive decline and conditions like Alzheimer’s disease and other dementias.
You might wonder: Does everyone’s gray matter shrink as they get older? Yes, brain volume changes over time are part of normal aging. But it’s also influenced by health factors, genetics, lifestyle, and underlying medical conditions. In my own practice, I’ve seen people in their 50s who have sharper memories than some 30-year-olds, which just shows that chronological age isn’t the only factor at play!
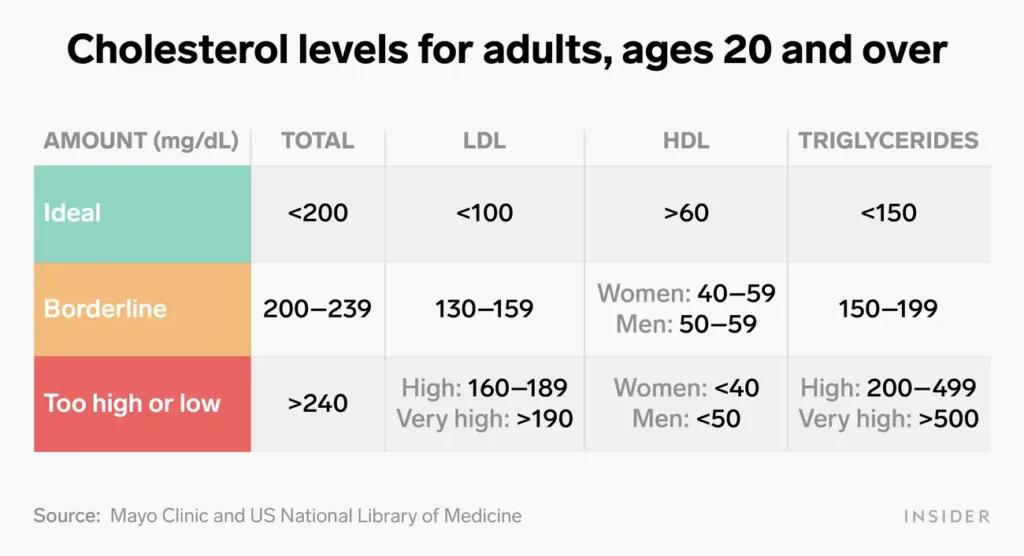
What Are Normal Cholesterol Levels?
HDL: Not Just Good, But Great?
HDL is often simplified as the “good” cholesterol because it picks up excess cholesterol from the bloodstream and takes it back to the liver, where it gets broken down and removed. Meanwhile, LDL (low-density lipoprotein) is considered the “bad” cholesterol because it can deposit cholesterol in your blood vessels, contributing to plaque build-up and atherosclerosis (a narrowing of the arteries). But this new study suggests there may be much more to HDL’s story.
- Small-Particle HDL Crossing the Blood-Brain Barrier
One reason smaller HDL particles might be so crucial is that they can potentially cross the blood-brain barrier—our brain’s “security system” that keeps harmful substances out. Larger particles may not make it into the brain as easily. Once there, small HDL particles could be acting as a sort of “cleanup crew,” removing bad cholesterol or toxic substances that threaten brain cells. - Cholesterol Efflux Capacity
The study mentioned “cholesterol efflux,” which is the ability of HDL to “scoop up” cholesterol from blood vessel plaques and bring it back to the liver. Imagine HDL as a kind of vacuum cleaner, searching for and sucking up the harmful cholesterol deposits that could lead to blockages. A higher capacity for this function means better removal of bad cholesterol—and possibly fewer damaging effects on the brain’s blood vessels. - Brain Volume Preservation
By measuring the participants’ brain MRIs over time, the researchers found that higher concentrations of these small HDL particles correlated with greater gray matter volume. That doesn’t automatically prove cause and effect—more studies are needed—but it’s certainly an exciting clue that improving small HDL particle function could help preserve brain health.
From the ER to Your Living Room: Why This Matters to You

I’ve spent many long nights in the ER with patients (and their worried families) who never expected to find themselves in a hospital bed, experiencing a stroke or concerning memory lapses. One moment, they’re out shopping or driving home from work, and the next, they realize they’re struggling to speak or recall details. These situations drive home the point that brain health is vital and often influenced by health conditions like high blood pressure, diabetes, and high cholesterol.
Seeing such scenarios repeatedly, I always talk about prevention in my family medicine practice. We discuss routine labs, lifestyle changes, and what new research might mean for them. Now, with this study from UT Southwestern, I’m even more motivated to spread the word about the importance of understanding your cholesterol profile—beyond just the standard total LDL and HDL numbers.
Ask yourself: When was the last time you had your cholesterol checked? Do you know your numbers, or is it just another line item on your lab results that you skim over without truly analyzing? Many of us feel relief when our doctor says, “Your HDL is in a healthy range,” but do we know if it’s actually doing what it’s supposed to do? This study suggests that function—how well your HDL particles are working—might be more important than the mere concentration of total HDL in your bloodstream.
Practical Tips: How Can You Nurture Your HDL?
You might be wondering, “How do I increase my small-particle HDL or improve HDL function?” While this research is still unfolding, we do know that there are established ways to improve your cholesterol profile and overall cardiovascular health. If you’ve spent any time with me in the ER or in the clinic, you’ve likely heard me preach about a few key strategies:
- Healthy Eating:
Focus on a diet that’s rich in whole foods, such as fruits, vegetables, whole grains, lean proteins, and heart-healthy fats (like those found in fish, nuts, and avocados). Limit processed, sugary, and fried foods. It might not sound revolutionary, but a balanced diet truly is foundational for better cholesterol levels. - Regular Physical Activity:
Exercise can help raise your HDL and lower your LDL. You don’t need to train for a marathon; consistency is key. Even brisk walking for 30 minutes most days of the week can help. Have you tried dancing around your living room while listening to your favorite tunes? Trust me, it’s both fun and effective! - Maintain a Healthy Weight:
Carrying excess body weight—especially around the midsection—can affect your cholesterol profile, blood pressure, and blood sugar. Even a modest weight loss of 5-10% of your body weight can lead to significant improvements in your labs. - Quit Smoking (If You Smoke):
Smoking lowers HDL levels and damages blood vessels. In my years in the ER, I’ve witnessed how quitting smoking can be one of the most powerful moves a person can make to protect both their heart and brain. - Limit Alcohol Consumption:
While some research suggests moderate alcohol intake could raise HDL, binge drinking or excessive intake can do far more harm than good. Know your limits, and if you don’t drink, there’s no need to start—other ways to improve HDL are safer and more effective. - Manage Chronic Conditions:
Conditions like diabetes, high blood pressure, and kidney disease can have a ripple effect on your cholesterol levels and your overall cardiovascular and brain health. Regular check-ups, medications as prescribed, and open communication with your healthcare provider can make a world of difference. - Consider Medications:
Statins are commonly prescribed to lower LDL, but there are other medication classes that can affect HDL. If you have a history of severely low HDL or other risk factors, talk to your doctor about whether medication could help you. While the research on medications specifically targeting HDL function is ongoing, your care team can give personalized recommendations based on your risk profile.
The Future of Brain Health: Why We’re Excited
One of the reasons this study is so groundbreaking is that it’s pointing the way toward more tailored and specialized measures of cholesterol health. Instead of just a broad “Your HDL is good,” we’re getting a more nuanced idea of which specific HDL particles—namely, the small ones—are helping protect the brain.
Additionally, Dr. Wanpen Vongpatanasin, one of the study’s authors, emphasized that simply looking at the concentration of HDL cholesterol may not reflect how well it’s functioning. This opens the door to new, more detailed testing methods in the future that look at the function and size of HDL. Imagine a day when your routine check-up includes a detailed analysis of your HDL subfractions and your provider can say, “Good news, your small-particle HDL is high and functioning great—your brain is in good hands!”
But we’re not quite there yet. It will take more research to confirm exactly how small-particle HDL crosses the blood-brain barrier and preserves brain cells. We also don’t know whether interventions specifically aimed at boosting small HDL will effectively slow cognitive decline. Yet, the optimism among the researchers is palpable—and for good reason! Any time we can pinpoint a mechanism that has the potential to protect us from the mental decline associated with aging, it’s a big deal.
A Personal Perspective
I’ve encountered countless middle-aged patients who are juggling careers, caring for aging parents, and raising kids—all while coping with their own health concerns. Cholesterol often becomes an afterthought until it’s flagged in a routine lab test. But considering the role it might play in our thinking, memory, and overall brain function, we can’t afford to ignore it.
In the ER, when a person shows up in a confused or disoriented state, we perform a thorough workup that looks at many factors—heart function, potential infections, medication side effects, and yes, even cholesterol levels. Sometimes patients say, “But my cholesterol isn’t that bad!” Yet, we know that even borderline cholesterol issues can contribute to long-term vascular changes that impact the brain. This new research simply confirms what many of us have suspected: Taking care of your cholesterol profile means more than just avoiding a heart attack; it might also be key to maintaining your independence and cognitive vitality.
As a family nurse practitioner, I make it a point to ask patients about any changes in memory or concentration, no matter how trivial they may seem. It’s part of a more holistic approach, one that looks at lifestyle, stress levels, sleep patterns, and nutrition. I often ask questions like, “Are you having trouble remembering the names of colleagues or clients you’ve known for years?” or “Do you find yourself more absent-minded than usual?” These questions not only help pinpoint potential issues early but also open the door to discussing how everyday habits—like diet and exercise—could be influencing both heart and brain health.
Food for Thought…
- How well do you really understand your cholesterol numbers?
- Are you just looking at your total HDL value, or have you considered the different subtypes?
- Could lifestyle changes you make today preserve not only your heart but also your mind in the years to come?
- Is it time for you to take your routine lab checks and follow-ups more seriously?
These questions are meant to spark a conversation between you and your healthcare provider. If you walk away from this article feeling a newfound sense of curiosity about the role of HDL in your brain health, then I’ve done my job as a nurse practitioner. And while science is still uncovering the nitty-gritty details, one thing remains abundantly clear: we all have the power to take small steps that can add up to substantial benefits for both body and mind.
Moving Forward

The journey to better health is always evolving. With each new study, our understanding of the human body becomes more refined, and this UT Southwestern research on HDL’s role in preserving brain volume is another exciting piece of the puzzle. As we learn more, we’ll hopefully have even better tools to identify those at higher risk of cognitive decline and to implement strategies—whether it be lifestyle changes, medications, or targeted interventions—to keep brains functioning at their peak.
In the meantime, keep up with regular check-ups, discuss any memory concerns with your provider, and continue focusing on well-rounded heart-healthy habits. By nurturing your HDL and overall cholesterol profile, you’re investing not just in your cardiovascular health, but possibly in your future cognitive health too.
So, the next time you find yourself thinking, “I need to watch my cholesterol,” remember that you might just be helping your brain stay sharp as well. As always, stay curious, stay informed, and stay proactive in your healthcare journey. If I’ve learned anything in my time in the ER and family clinic, it’s this: prevention and early detection really do save lives—and, apparently, they just might save our precious gray matter as well.