by Todd Dunn
Color, clarity and size (quantity) isn’t just for diamonds. It is also how your urine output is assessed after surgery and when you are critically ill. Why, because urine provides insights on how your kidneys are functioning. Not only do your kidneys clean the blood (and remove “the bad stuff” through urine), they also impact your blood pressure and all vital organ function. When your output of pee decreases it may be an early indication that your kidneys are malfunctioning.
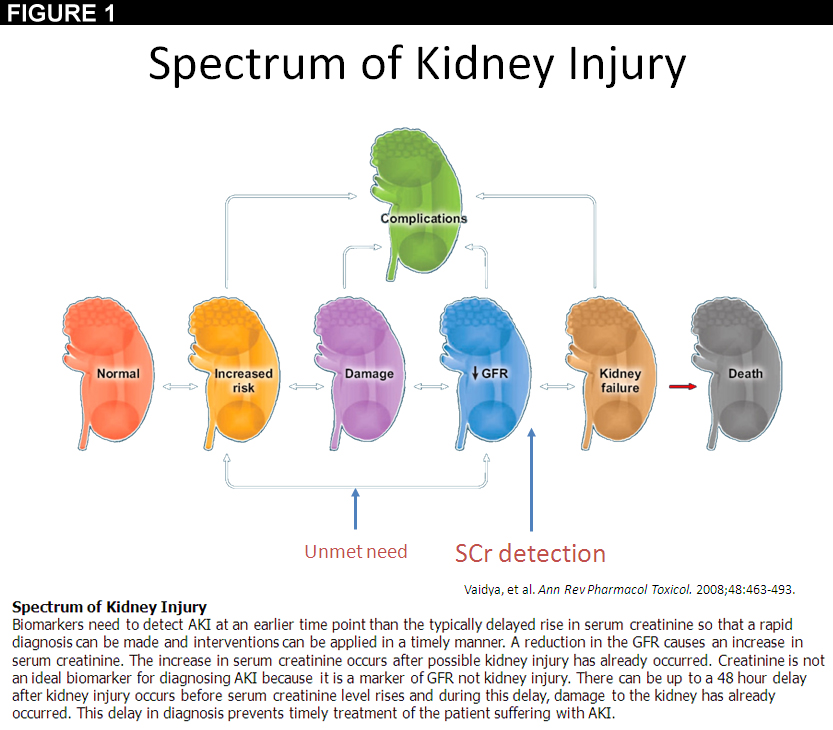
When your kidneys malfunction it is diagnosed as acute kidney injury (AKI) which is categorized in “stages” the stages have to do with how long you go without producing a minimal amount of pee for your size (0.5mL/kg/hr) or how elevated levels of serum creatine show up in your blood (more on that later). As the “stages” of AKI progress the damage to your kidneys becomes greater and your risk of increased complications and even death escalates.
Kidneys are a vital organ that are primarily monitored by looking at a patient’s pee (or blood) when they are very sick. What you may not know is that although it is outlined in the guidelines that the amount you pee should be assessed every hour with accuracy to monitor kidney function, the reality is that there is a nursing staffing crisis and even in a well staffed hospital the probability that a nurse will be able to monitor, measure and chart your pee with great accuracy every hour during their 10-12 hour shift is low.
In fact, each year 4.9 million people get diagnosed with an acute kidney injury while in the hospital. That is a person every 6.5 seconds. We would NEVER accept a heart getting damaged in any way every 6.5 seconds in the hospital!
Why is this happening, let’s walk through a scenario. A patient is lying in the intensive care unit (ICU) bed with a foley catheter. You are at their bedside and notice that there is pee in the collection bag and some that appears to be “stuck” in the catheter tubing. The pee that is stuck in the tubing is actually due to the design of the foley catheter. Think about the catheter as a hose. All hoses get kinks in them and water stops moving. There are times when a loop happens in the catheter and urine stops flowing. In order to report how much pee you have produced the nurse “milks” the catheter to move the pee in the tube into the collection bag, they then drain the bag, measure in a cylinder the amount of pee collected, and then chart how much urine you have produced. According to “The Work of Adult and Pediatric Intensive Care Unit Nurses,” an article published in Nursing Research, nurses perform over 125 tasks per hour. No wonder it is tough for them to monitor how much pee you are producing every hour, and it is highly likely that the early warning signs your kidneys are sending (low output of urine) are often missed.
The current standard of care is sabotaging the clinician’s ability to protect your kidneys. First, because of the risk of developing a catheter urinary tract infection (CAUTI) which not only prolongs your stay in the ICU, but also costs the hospital money, Therefore, your foley catheter is removed as soon as possible…some may argue too soon, because they lose insights (even as marginal as they are) on how much urine your kidneys are producing. The blood test that is ordered to see look at your serum creatinine to determine if your kidneys are functioning is described by many as a “lagging indicator” because the results are often delayed as much as 24-72 hours and elevated serum creatinine is a result of the fact that your kidney function is already compromise.
The key challenge with kidney care in the hospital today is that clinicians don’t have access to an automated device designed to monitor the kidneys similar to what is used to monitor the heart and lungs! Standard of care is not providing early, accurate and reliable information for clinicians to act on.
I wonder how many patients are aware of the risk, when they enter the hospital, that they might walk out with compromised kidney function that can lead to increased mortality within one year of their hospital stay? I often think, would Providers rely on urine output differently if it were as accurate and reliable as a patient’s blood pressure that shows up on the monitor, and that integrating this single data point into your patient care bundles could reduce the incidence of AKI?
We can do better! My job as an innovator is to focus on care transformation by serving other people and awakening possibilities in what we can collectively do to improve the cost and quality of healthcare. With that missionI went on a hunt and found a solution to help protect kidneys: the Accuryn monitor from Accuryn Medical.We can do better! My job as an innovator is to focus on care transformation by serving other people and awakening possibilities in what we can collectively do to improve the cost and quality of healthcare. With that missionI went on a hunt and found a solution to help protect kidneys: the Accuryn monitor from Accuryn Medical.
Accuryn enables clinical teams to have a digital understanding of the kidney just like we have for the heart. It makes caring for the kidneys easier. Accuryn’s device counts every drop of urine the kidneys produce, while keeping urine flowing through the tubing which decreases the infection risk associated with current foley catheters. The accurate data can automatically populate in the patient’s health record, and gives clinical teams a notification when the kidneys are under distress (AKI Stage alerts at the bedside). The future of kidney care is here. Let’s get the word out. Feel free to reach out to me if you want to know more about why I drove to find a better way to make it easy to do the right thing and hard to do the wrong thing for patients’ kidneys.
Todd Dunn is the Vice President of Enterprise Innovation