By Alice Benjamin, MSN, ACNS-BC, FNP-C
Imagine seeking care for your child, who is struggling to align their physical appearance with their gender identity. You’ve done the research, consulted with experts, and are ready to take the next steps. But when you sit down with your healthcare provider, you’re told they can’t help—not because they don’t want to, but because the law has tied their hands.
This is the reality in Texas and other states where gender-affirming care for minors has been banned. For healthcare providers, this isn’t about personal beliefs or lack of compassion—it’s about navigating a growing minefield of legal and professional risks.
Doctor in white coat with handcuffs holds stethoscope standing on light background. Professional medic worker arrested for medical error
For patients and their families, understanding what gender-affirming care involves and why providers are caught in the crossfire is key to navigating this complex and challenging landscape. Here’s what you need to know about the care, the laws restricting it, and what you can do if you find yourself unable to access the support you need.
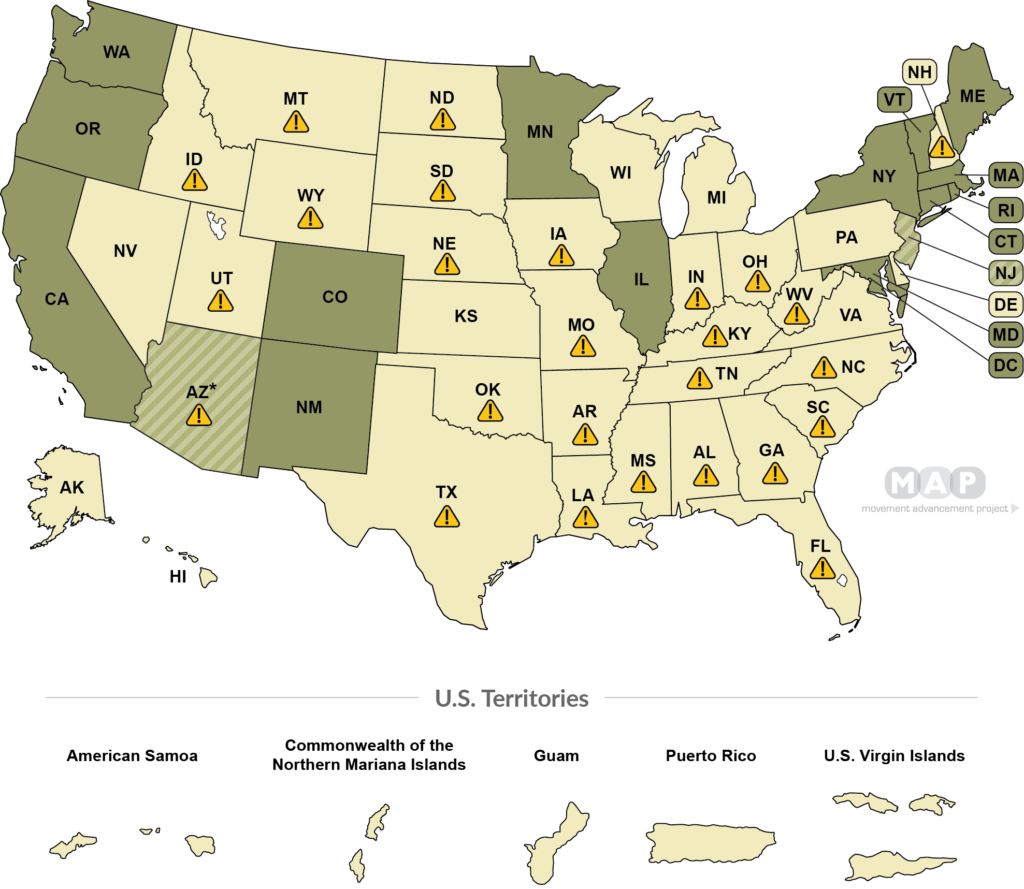 Movement Advancement Project. “Equality Maps: Transgender Healthcare ‘Shield’ Laws.” www.mapresearch.org/equality-maps/healthcare/trans_shield_laws. Accessed 11/24/2024.[/caption]
Movement Advancement Project. “Equality Maps: Transgender Healthcare ‘Shield’ Laws.” www.mapresearch.org/equality-maps/healthcare/trans_shield_laws. Accessed 11/24/2024.[/caption]
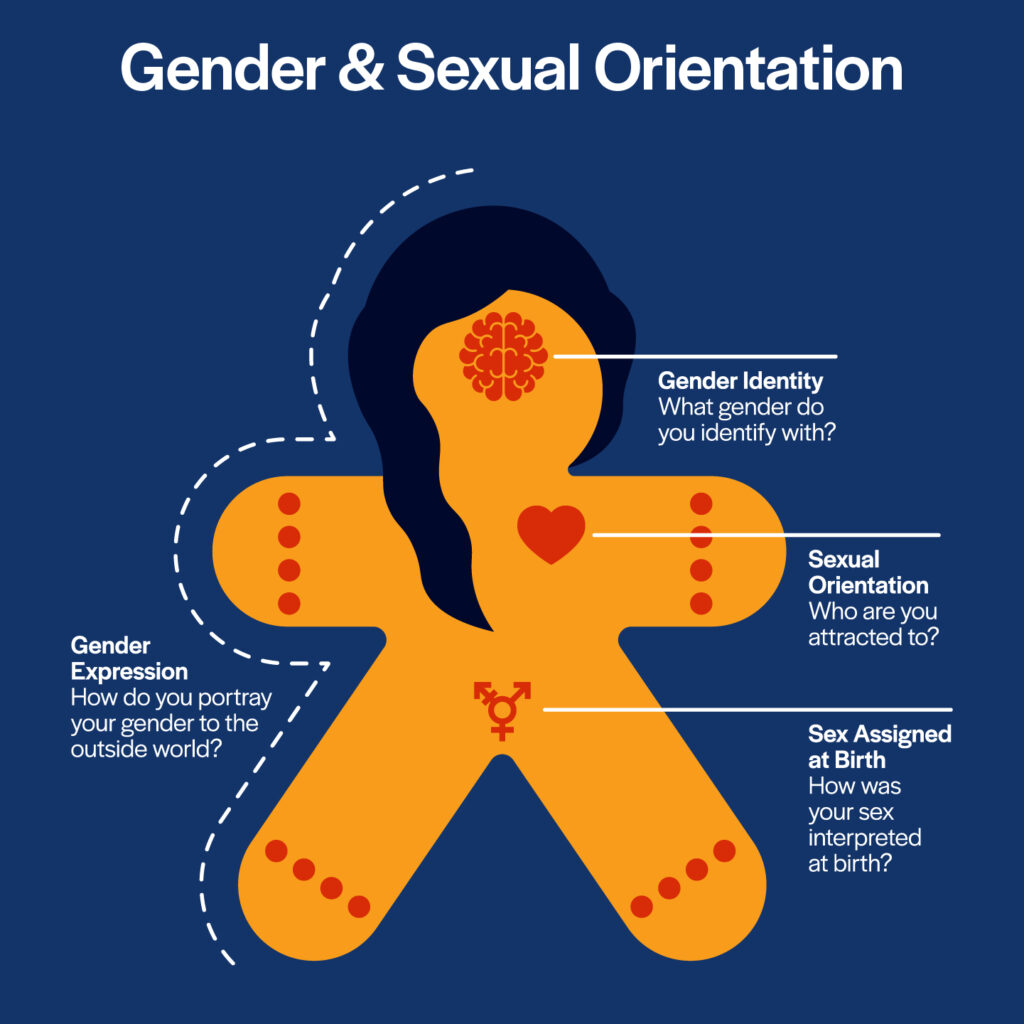
What Is Gender-Affirming Care?
Gender-affirming care encompasses a range of medical, psychological, and social interventions designed to help individuals align their physical characteristics and lived experiences with their gender identity. It’s rooted in evidence-based practices and supported by major medical organizations such as the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the World Professional Association for Transgender Health (WPATH).
Key Components of Gender-Affirming Care
Social Transitioning: This is often the first step, especially for children. It involves non-medical changes, such as using a preferred name and pronouns, allowing the individual to dress in ways that align with their gender identity, and creating inclusive environments.
Puberty Blockers: These are medications that temporarily pause puberty, preventing the development of secondary sex characteristics like facial hair or breast development. This is not a permanent measure but a way to give young people more time to explore their gender identity.
Hormone Therapy: This involves the use of testosterone or estrogen to help individuals develop physical traits that align with their gender identity. It’s typically reserved for older teens and adults after thorough evaluations.
Mental Health Support: Counseling and therapy are crucial components of gender-affirming care, helping individuals and their families cope with gender dysphoria and the social challenges that often accompany it.
Surgical Interventions: While surgeries are a part of gender-affirming care, they are exceedingly rare for minors. When performed, they are typically reserved for adults or older teens who have undergone extensive evaluations and have a strong support system in place.
What Gender-Affirming Care Isn’t
There are numerous myths and misconceptions surrounding gender-affirming care. To clarify:
It’s Not Rushed or Careless: Decisions about gender-affirming care are made over time, with careful evaluation by medical and mental health professionals. Families are deeply involved in the process.
It’s Not Harmful: Research consistently shows that gender-affirming care significantly reduces rates of depression, anxiety, and suicidal ideation among transgender individuals. It’s an essential component of their overall health and well-being.
It’s Not a One-Size-Fits-All Solution: Every person’s journey is unique, and the care provided is tailored to their specific needs, age, and circumstances.
Why Is Gender-Affirming Care Sought?
Gender-affirming care is often sought to address gender dysphoria, a condition where a person’s assigned sex at birth does not align with their gender identity, leading to significant distress. Untreated gender dysphoria can result in severe mental health challenges, including depression, anxiety, and suicidal ideation.
For children and adolescents, early interventions like social transitioning or puberty blockers can provide a sense of relief and stability, helping them navigate their identity with confidence. For adults, interventions like hormone therapy or surgeries can improve quality of life, helping them live authentically and without the constant distress of dysphoria.
Families typically pursue gender-affirming care after thorough consultations with mental health professionals, pediatricians, and specialists, ensuring that the decisions made are in the best interests of their loved one.
How Laws Restrict Gender-Affirming Care
In recent years, a wave of legislation has targeted gender-affirming care, particularly for minors. In Texas, Senate Bill 14 (SB 14) prohibits the use of puberty blockers, hormone therapies, and surgeries for individuals under 18. The law also bans providers from referring patients for these treatments elsewhere.
What Are the Risks for Providers?
Under these laws, providers face significant consequences if they are found to have violated restrictions:
- Loss of Licensure: Providers risk losing their ability to practice medicine or nursing in their state.
- Financial Penalties: Violations can result in hefty fines.
- Criminal Charges: In some cases, providers may face criminal prosecution, which could lead to imprisonment.
Real Examples of Providers Caught in the Crossfire
In Texas, three physicians have been sued by Attorney General Ken Paxton for allegedly violating SB 14:
- Dr. May Lau: A Dallas-based pediatrician is accused of prescribing hormone treatments to minors and now faces potential fines and license revocation.
- Dr. Hector Granados: An El Paso pediatric endocrinologist is alleged to have provided puberty blockers to minors under a diagnosis of precocious puberty to circumvent the law.
- Dr. M. Brett Cooper: Another Dallas physician has been sued for prescribing gender-affirming care, becoming the third target of lawsuits in the state.
These legal actions highlight the difficult position providers are in, as they try to balance their ethical obligations to patients with the legal risks of offering care.
What Can Patients and Families Do?
If you or a loved one is affected by these laws, there are still steps you can take to advocate for and access care:
1. Learn the Laws in Your State
Understand the specific restrictions in your state and what care options are still legally available.
2. Open Communication with Providers
Discuss your concerns with your healthcare provider. While they may be limited by the law, they can often help with referrals to advocacy organizations or provide general guidance.
3. Explore Out-of-State Options
Seek care in states where gender-affirming treatments are still legal. Many organizations maintain directories of supportive providers across the country.
4. Use Telehealth Services
Some telehealth platforms can connect you with providers in states where care is legal. However, be aware of any regulations that may limit telehealth access.
5. Connect with Advocacy Groups
Organizations like The Trevor Project, Lambda Legal, and GLAAD offer resources, legal guidance, and support for individuals navigating these challenges.
6. Raise Awareness and Advocate for Change
Share your story, join advocacy campaigns, and engage with lawmakers to push for evidence-based, compassionate policies.
Why This Matters
For healthcare providers, laws like SB 14 create a heartbreaking conflict between their professional obligations and the risk of legal and professional consequences. For patients and families, these laws can feel like an insurmountable barrier to care.
Understanding the realities of gender-affirming care, the laws restricting it, and the steps you can take to advocate for your needs is essential in this challenging time. Together, patients, families, and providers can work toward a future where evidence-based care is accessible to all who need it.